Lab 3 - Spinal Cord & Brainstem: Surface and Sectional Anatomy
|
| Reading: |
|
|
| Coursera Media: |
|
|
Lab 3 Protocols
- Spinal Cord
- Learning objective: to recognize the principal features of the spinal cord, including the longitudinal organization of spinal segments and internal distinctions among levels.
- Specimens: one spinal cord specimen available for demonstration purposes
- Activities:
- Open the Laboratory Guide to Figure 2.4 and visit the demonstration spinal cord specimen.
- Identify the cervical and lumbosacral enlargements, and the thoracic and sacral regions.
- Identify dorsal and ventral roots.
- Differentiate the dura mater from arachnoid mater, and identify denticulate ligaments
- Identify the posterior and anterior spinal arteries, and draining veins
- Open the Laboratory Guide to Figure 2.7 and the chart on following page, and open the histological atlas of the brainstem and spinal cord (“Brainstem Cross-Sectional Atlas”) in Sylvius4 Online (see the Sylvius Self-Study Exercise—Medullary Surface)
- Find each of the features listed in the chart and described in the text as you can on the sectional, histological views of the human spinal cord. (Do Challenge 3.1).
- Medulla oblongata
- Learning objective: to recognize the principal features of the medulla oblongata as seen from the
surface, including the attachments of cranial nerves VI-X and XII (and XI).
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.9 and its corresponding chart.
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated just as easily in hemi-brains that were sectioned in the mid-sagittal plane. You
may wish to refer the actual specimens to the models available in the lab for comparison and/or to
the brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Medullary Surface).
- Pons
- Learning objective: to recognize the principal features of the pons as seen from the surface, including
the attachments of cranial nerves V and VI-VIII.
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.10 and its corresponding chart.
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated just as easily in hemi-brains that were sectioned in the mid-sagittal plane. You
may wish to refer the actual specimens to the models available in the lab for comparison and/or to
the brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Pontine Surface).
- Midbrain
- Learning objective: to recognize the principal features of the midbrain as seen from the surface,
including the attachments of cranial nerves III & IV.
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.11 and its corresponding chart.
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated best in hemi-brains that were sectioned in the mid-sagittal plane. You may wish
to refer the actual specimens to the models available in the lab for comparison and/or to the
brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Midbrain Surface).
- Do the brainstem Challenges
- Learning objective: to recognize the relation between major external features of the brainstem, including the cranial nerves, and internal gray matter and white matter structures in each embryological division.
- Resources: whole brains, mid-sagittal hemispheres, or brainstem models; Sylvius4 Online
- Activities:
- Work through Challenges 2.2−2.4 by referring to the charts and figures associated with descriptions of various sections through the medulla, pons and midbrain. Find each of the features listed in the charts and described in the text as you can on actual specimens.
- Identify internal features of the brainstem that account for distinctive external features of each embryological subdivision; refer to the Brainstem Atlas in Sylvius4 Online for additional sections and annotations.
- Examine slabs through human brainstem specimens
- Learning objective: to recognize the principal features of the brainstem that are visible with the unaided eye, including major gray matter and white matter structures in each embryological division.
- Specimens: whole brain slabs or gross sections cut through the brainstem
- Activities:
- Repeat Challenges 2.2−2.4 using gross sections through the human brainstem, referring to the charts and figures associated with the text and the Brainstem Atlas in Sylvius4 Online.
- Find as many of the visible gray and white matter features listed in the chart and described in the text as you can on actual specimens of the human brainstem.
Introduction

The central nervous system interacts with the outside world through primary sensory neurons, which convey information from the body or its environment into the brain and spinal cord, and motor neurons, which activate striated muscles and modulate the activity of cardiac and smooth muscles and glands (Figure 2.1). The cell bodies of primary sensory neurons lie outside the CNS in dorsal root ganglia or cranial nerve ganglia. Each neuron gives rise to a peripheral process, which receives information either directly or through association with receptors, and a central process, which enters the CNS and forms synapses with second order neurons. The cell bodies of somatic motor neurons lie in clusters called cranial nerve nuclei within the CNS and give rise to axons that innervate striated muscles in the body or head. Other motor neurons form part of the autonomic nervous system; they reside outside of the central nervous system and innervate cardiac muscle, smooth muscle or glands.
Of chief importance in understanding the organization of the brainstem and spinal cord is knowledge of what is localized in each embryological subdivision and in any transverse section from any level. This is a significant challenge for every student of neuroanatomy and the first step toward mastery of this knowledge is to recognize the external features of each brainstem subdivision, including the associated cranial nerves, and each major level of the spinal cord.
In this laboratory experience, you will appreciate the relationship between the nerves formed by the axons of primary sensory and motor neurons in the brainstem (and spinal cord). There are numerous bumps and furrows along the length of the brainstem and spinal cord that provide visible landmarks on their surfaces; you will eventually understand the organization of internal structures that account for these bumps and furrows. For today, one challenge will be to learn the relation of the cranial nerves and spinal nerve roots to these superficial features of the brainstem and spinal cord. In doing so, you will learn the gross features that characterize the three embryological subdivisions of the brainstem and the spinal cord.
But before beginning a detailed study of the internal anatomy of the brain, it will be helpful to familiarize yourself with some common conventions that are used to describe the deep structures of the central nervous system.
Terminology and general principles

The next few sections contain definitions and illustrations of some commonly used neuroanatomical terminology. They may be useful for reference as you study the material in this and the following laboratory sessions.
The simplest classification of central nervous tissue is white matter and gray matter (see Figure 2.2) The gray matter (so-named because it looks grayish in fresh specimens, as you have already seen) is made up of neuronal cell bodies, their dendrites, and the terminal arborizations of both local axons and those from distant sources. The dendrites and the axons that form synapses with them are sometimes referred to as “neuropil.” The white matter is made up of the axons that connect separated areas of gray matter. The myelin that ensheathes many of these axons gives the white matter its glistening white appearance. Note that an individual neuron can contribute to both gray and white matter. Axons projecting from one part of the brain to another usually group together in bundles. Likewise, neurons that serve similar functions often form clusters.
Terms used to refer to gray matter
Column
Cortex (plural: cortices; L., bark)
Ganglion (plural: ganglia; Gr., swelling)
Layer
Nucleus (plural: nuclei)
Terms used to refer to white matter
These five terms are used to refer to bundles of axons:
Column
Fasciculus (L., fascia, band or bundle)
Funiculus (L., funis, cord)
Lemniscus (L. from Gr., lemniskos, fillet, ribbon)
Tract
These terms also refer to bundles of axons, but they are usually used to refer to bundles that can be seen from the surface of the brain:
Brachium (L., arm)
Peduncle (L., pes, foot, stalk)
These terms refer to the crossing of axons from one side of the CNS to the other. A commissure contains axons crossing from one location to its counterpart on the other side. A decussation contains axons that travel to a contralateral location in a non-corresponding region of the central nervous system.
Commissure (L., joining together)
Decussation (L., decussare, to cross in the form of an "X")
Many nuclei and tracts in the central nervous system are much longer than they are wide, calling to mind a column.
(Note that the word 'column' is used to refer to both white matter and gray matter.) Although the terms that refer to
white matter structures are not used interchangeably, they all refer to essentially the same constituent—axons (often in
a compact bundle) connecting one area of gray matter to another.
You will also encounter the following terms used to refer to general regions of the central nervous system:
tectum (L., roof) — used to refer to brainstem structures located dorsal to the ventricular system. In mammals, this
term has become synonymous with the dorsal midbrain.
tegmentum — this term refers to structures that form the core of the brainstem (e.g., as shown in this figure). It can be thought of
(very loosely) as the part of the brainstem that is most like the spinal cord in the sense that the cell groups in the
tegmentum have functions similar to those of cell groups in the spinal cord. For the most part, the structures that lie
outside the tegmentum have no counterparts in the spinal cord.
base — the ventral aspect of the brain. The term ‘basal’ is synonymous with ‘ventral.’ For example, the bulbous portion of the pons is in the base of the pons (“basilar pons” or “basis pontis”), which is ventral to the tegmentum.
floor, wall — usually used with respect to structures that bound the ventricles (e.g., the floor of the fourth ventricle
corresponds to the part of the pons and medulla that forms the ventral boundary of the ventricle).


From the viewpoint of clinical practice, the most important general principle of organization in the central nervous system is that each CNS function (e.g., perception of sensory stimuli, control of motor behavior) involves groups of neurons—interconnected through synapses—that are spatially distributed throughout several CNS subdivisions. Groups of neurons that together subserve a particular function are called a ‘system’; for example, there are the visual, motor, and somatic sensory systems. The structures containing the neurons and axons of a particular system are collectively referred to as a ‘pathway’. (The term ‘system’ has a functional connotation, whereas the term ‘pathway’ refers to the structures involved.) Two important pathways are illustrated in Figure 2.3; components of these two pathways will be identified in sectional views of the brainstem and spinal cord in subsequent sections of this chapter.
Note that receptors and muscles on the right side of the body are represented in the left side of the forebrain—a fact will be emphasized repeatedly over the next few weeks. Knowledge of the crossing of sensory and motor pathways as they ascend or descend provides critical information to the clinician who is localizing neurological lesions.
If damage to the CNS at every level gave rise to exactly the same signs and symptoms, it would not be worthwhile for you to learn the details of neuroanatomy. However, as neurologists and neuroscientists recognized long ago, the neurons involved in specific functions occupy specific locations in the central nervous system. Even those systems that are represented in multiple subdivisions bear different physical relationships to one another from one subdivision to the next. Because neurons that subserve specific functions occupy specific locations, the combinations of neurological signs and symptoms exhibited by particular patients often provide detailed information about the location of damage in the CNS (see Appendix 5).
The spinal cord
- Learning objective: to recognize the principal features of the spinal cord, including the longitudinal organization of spinal segments and internal distinctions among levels.
- Specimens: one spinal cord specimen available for demonstration purposes
- Activities:
- Open the Laboratory Guide to Figure 2.4 and visit the demonstration spinal cord specimen.
- Identify the cervical and lumbosacral enlargements, and the thoracic and sacral regions.
- Identify dorsal and ventral roots.
- Differentiate the dura mater from arachnoid mater, and identify denticulate ligaments
- Identify the posterior and anterior spinal arteries, and draining veins
- Open the Laboratory Guide to Figure 2.7 and the chart on following page, and open the histological atlas of the brainstem and spinal cord (“Brainstem Cross-Sectional Atlas”) in Sylvius4 Online (see the Sylvius Self-Study Exercise—Medullary Surface)
- Find each of the features listed in the chart and described in the text as you can on the sectional, histological views of the human spinal cord. (Do Challenge 2.1).
 
The spinal cord extends caudally from the brainstem, running from the medullary-spinal junction at about the level of the first cervical vertebra to about the level of the first lumbar vertebra (Figure 2.4). The vertebral column (and the spinal cord within it) is divided into cervical, thoracic, lumbar, sacral, and coccygeal regions. The peripheral nerves (called the spinal or segmental nerves) that innervate much of the body arise from the spinal cord’s 31 pairs of spinal nerves. On each side of the midline, the cervical region of the cord gives rise to eight cervical nerves (C1–C8), the thoracic region to twelve thoracic nerves (T1–T12), the lumbar region to five lumbar nerves (L1–L5), the sacral region to five sacral nerves (S1–S5), and the coccygeal region to one coccygeal nerve. The segmental spinal nerves leave the vertebral column through the intervertebral foramina that lie adjacent to the respectively numbered vertebral body (with the C1 nerve exiting above the first cervical vertebra and the C2 nerve exiting below it). Sensory information carried by the afferent axons of the spinal nerves enters the cord via the dorsal roots, and motor commands carried by the efferent axons leave the cord via the ventral roots. Once the dorsal and ventral roots join, sensory and motor axons (with some exceptions) travel together in the segmental spinal nerves (Figure 2.5). (See Appendix 5 for a reminder of the typical dermatomal map).
Two regions of the spinal cord are enlarged to accommodate the greater number of nerve cells and connections needed to process information related to the upper and lower limbs. The spinal cord expansion that corresponds to the arms is called the cervical enlargement and includes spinal segments C3–T1; the expansion that corresponds to the legs is called the lumbar enlargement and includes spinal segments L1–S2 (see Figure 2.4B). Because the spinal cord is considerably shorter than the vertebral column (see Figure 2.4A)., lumbar and sacral nerves run for some distance in the spinal canal before emerging, thus forming a collection of nerve roots known as the cauda equina. This region is the target for an important clinical procedure called a “lumbar puncture” that allows for the collection of cerebrospinal fluid by placing a needle into the space surrounding these nerves to withdraw fluid for analysis. In addition, local anesthetics can be safely introduced to produce spinal anesthesia; at this level, the risk of damage to the spinal cord from a poorly placed needle is minimized.
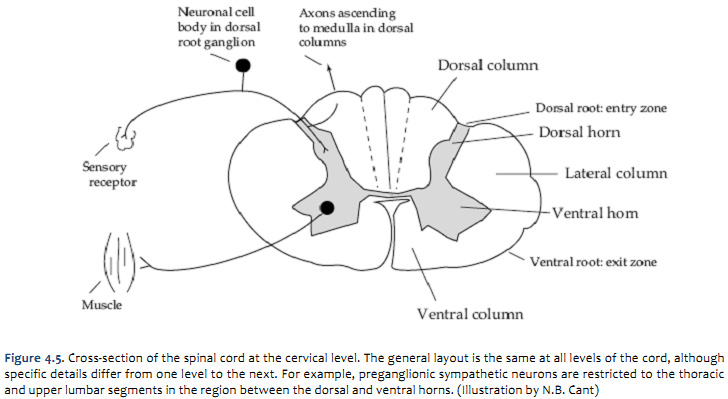
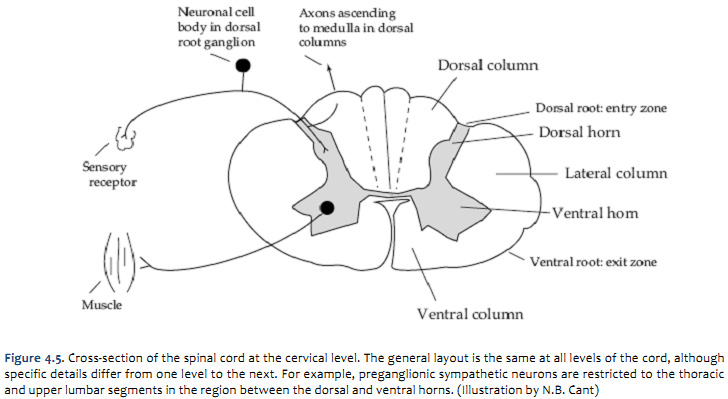
Internal anatomy of the spinal cord
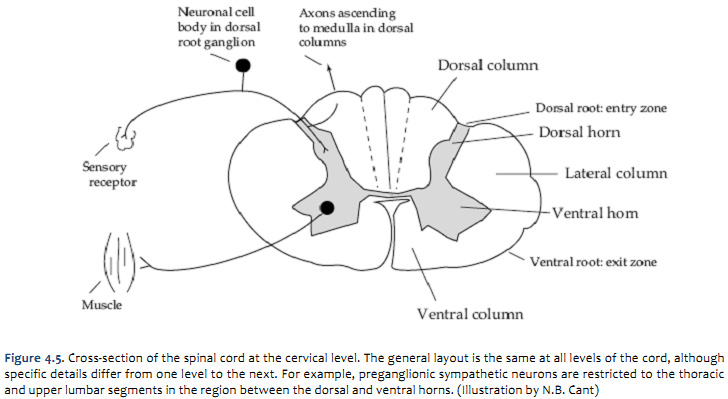 
The following discussion of the internal anatomy of the spinal cord will introduce some of the general principles of organization that also hold true for the brainstem. A cross-section through the spinal cord is illustrated schematically in Figure 2.6 and 3.4. The gray matter forms the interior of the spinal cord; it is surrounded on all sides by the white matter. The white matter is subdivided into dorsal (or posterior), lateral, and ventral (or anterior) columns. Each of these columns contains bundles of axons related to specific functions. For example, the lateral columns are made up partly of axons that travel from the cerebral cortex to form synapses with motor neurons in the ventral horn. The dorsal columns carry much of the ascending sensory information from mechanoreceptors (more on these long pathways in later sessions).
The gray matter of the spinal cord is divided into dorsal and ventral (or posterior and anterior) ‘horns.’ The dorsal horn is the part of the gray matter that receives sensory information entering the spinal cord via the dorsal roots of the spinal nerves. The ventral horn contains the cell bodies of lower motor neurons that send their axons out via the ventral roots to terminate on striated muscles. Thus, one important general rule of organization is that neurons in the spinal cord that process sensory information are spatially separate from motor neurons. (See Figure A6 and Table A1 of Neuroscience, 5th Ed., for more detail on the internal organization of spinal gray matter.)
As seen earlier, the inputs and outputs of the spinal cord are arranged segmentally into the 31 pairs of spinal nerves (Figure 2.4). However, the gray matter of the spinal cord is not obviously segmented. It can be thought of as continuous columns (ventral horn) and layers (dorsal horn) of cells that run the length of the cord, with important differences in the size of the dorsal and ventral horns at different levels. The dorsal and ventral horns are largest where they supply the upper and lower limbs, because there are significantly greater numbers of outgoing and incoming nerve fibers at those levels. There is also variation along the length of the cord in the number of fibers in the columns of white matter (and, therefore, in their relative size). The amount of white matter is greatest at cervical levels and least at sacral levels. This is because ascending and descending fibers from and to all levels must pass through the cervical cord.
| Challenge 3.1—internal anatomy of the spinal cord
With reference to Figure 2.6, 2.7, and 2.8 and the chart below, carefully inspect the internal features of the spinal cord that are present in each segment, as well as those that are different (or present in only in one segment). To complete this challenge, spend some time browsing the spinal cord sections in Sylvius4, and find each of the internal features identified across the upper row in the chart below in the Sylvius4 spinal cord. |
Chart 2-1 |
Internal features |
Spinal cord segment |
Dorsal horn |
Lateral horn |
Ventral horn |
White matter |
Gracile tract |
Cuneate tract |
Lateral corticospinal tract |
Ventral corticospinal tract |
Anterolateral system |
Cervical segments (8) |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0000.gif)
|
+++++ |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0001.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0002.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0003.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0004.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0005.gif)
|
Thoracic segments (12) |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0006.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0007.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0008.gif)
|
++++ |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0009.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0010.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0011.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0012.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0013.gif)
|
Lumbar segments (5) |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0014.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0015.gif)
|
+++ |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0016.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0017.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0018.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0019.gif)
|
Sacral segments (5) |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0020.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0021.gif)
|
++ |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0022.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0023.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0024.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0025.gif)
|
Coccygeal segment (1) |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0026.gif)
|
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0027.gif)
|
+ |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0028.gif)
|
-- |
-- |
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0029.gif)
|
![Description: C:\Documents and Settings\white033\Local Settings\Temporary Internet Files\Content.IE5\010AFA8B\MC900442153[1].png](https://brain.oit.duke.edu/lab05/lab05_clip_image002_0030.gif)
|
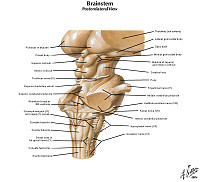
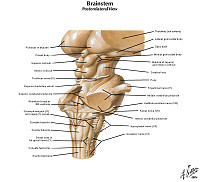
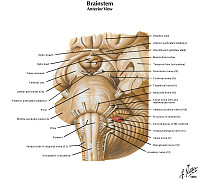
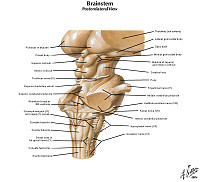
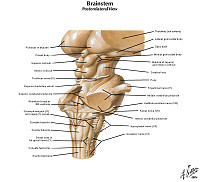
Surface anatomy of the brainstem
Unlike the spinal cord, which is relatively similar in appearance along its length, the brainstem looks very different from one part to another. The cranial nerves are not regularly arrayed like the spinal nerves, and there are many curious bumps and lumps along the surface of the brainstem that have no counterparts in the spinal cord. The following description of the surface appearance of each subdivision is intended to prepare you for the discussion of the intrinsic anatomy of the brainstem that follows later in this chapter. As you work through the descriptions in the text, as usual, you will be responsible for the terms in bold. A clear picture of the surface topography of the brainstem should help you to understand why sections through each level appear as they do.
We’ll begin working our way through the brainstem from caudal to rostral, starting with the medulla oblongata (or simply, the “medulla” for short).
Medulla
- Learning objective: to recognize the principal features of the medulla oblongata as seen from the
surface, including the attachments of cranial nerves VI-X and XII (and XI).
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.9 and its corresponding chart.
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated just as easily in hemi-brains that were sectioned in the mid-sagittal plane. You
may wish to refer the actual specimens to the models available in the lab for comparison and/or to
the brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Medullary Surface).
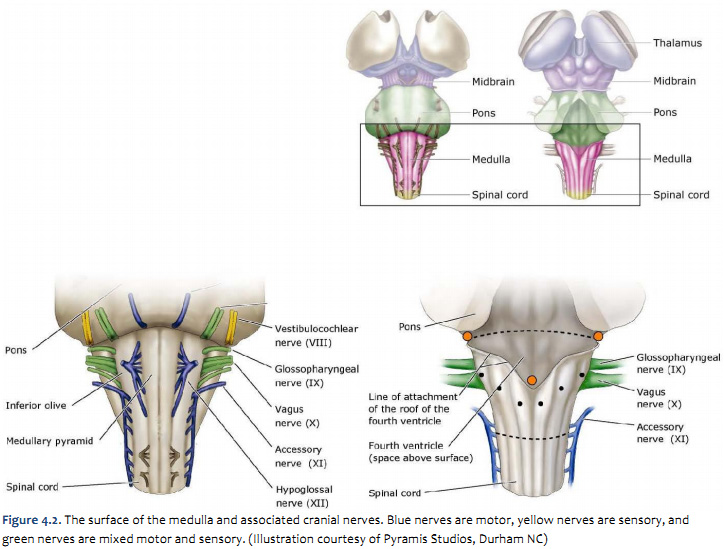
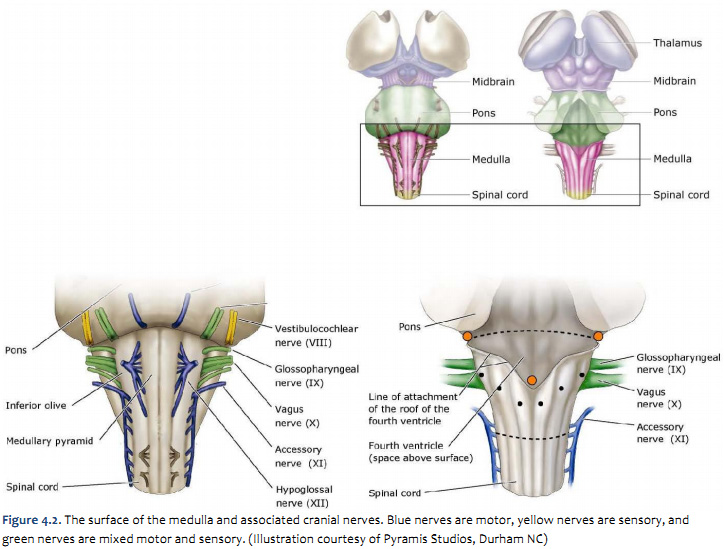
The medulla is bounded caudally by the spinal cord and rostrally by the pons. Features that characterize its surface are illustrated in Figure 2.9 (see also Netter 108A, 108B, 109A, and 109B). This illustration shows the key features of the medulla that are visible on its external surface; these include cranial nerves VI-X & XII, and a set of distinctive bumps, bulges and furrows. Actually, cranial nerves VI-VIII are more properly associated with the pons, since these nerves originate or terminate in cranial nerve nuclei (gray matter) that are localized mostly to the caudal pons. However, these three nerves exit at the ventral junction of the pons and medulla and it is appropriate to consider them here first.
On the ventral surface, bumps formed by fiber tracts known as the medullary pyramids sit next to the midline on each side. Lateral to the pyramids are bumps known as the olives formed on each side by a paired large nucleus in the medulla, called the inferior olivary nucleus (a nucleus that you will see in cross-sectional views of the medulla below). These two structures are critical to appreciate for reasons that will be discussed when motor control systems in the brain are considered. For now, they are useful landmarks for recognizing the rootlets of cranial nerve XII, the hypoglossal nerve, which emerge from the medulla between the pyramid and the olive. Cranial nerves IX, the glossopharyngeal nerve, and X, the vagus nerve, also connect to the brainstem in the medulla, although they do so more laterally than nerve XII; in fact, they connect just lateral to the olive. (Cranial nerve XI does not really connect to the medulla; it is made up of fibers that exit mainly from the spinal accessory nucleus of the upper cervical spinal cord and enter the cranium through the foramen magnum.)
The dorsal surface of the medulla is characterized by a series of longitudinal swellings (marked by the black dots in Figure 2.9 (see also Netter 108A, 108B, 109A, and 109B); don’t be concerned with their names). The important fact to note is that each of the swellings appears to be a continuation of a similar swelling on the dorsal surface of the spinal cord; however, the ones along the surface of the medulla are somewhat larger and more bulbous. Like the olives, these bumps indicate the outward bulging of gray matter structures that you will locate in sections through the caudal medulla; for now, let’s simply say that these structures in the caudal medulla are critical for the passage of somatic mechanosensory signals from the spinal cord to higher levels of processing in the forebrain.
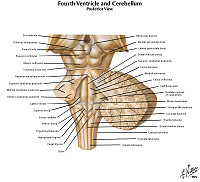
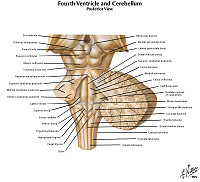
The most inferior portion of the medulla (the part near the spinal cord) is ‘closed,’ meaning that there is no fourth ventricle (only a central canal, continuous with that of the spinal cord). The fourth ventricle begins to open about halfway up the medulla and extends through the pons. The thin ‘roof’ of the fourth ventricle is not illustrated, and you are looking down into the ‘floor’ of the ventricle. The roof of the ventricle is made up only of ependymal cells, connective tissue (pia) and blood vessels. It contains three openings through which the cerebrospinal fluid that is produced in the ventricles escapes into the subarachnoid space. The approximate locations of the openings, known as the median and lateral apertures (or the foramen of Magendie and the foramina of Luschka, respectively), are indicated by orange dots in Figure 3.10 (see also Netter 108A, 108B, 109A, and 109B). The (pink) chart below lists these features and provides some additional localizing information. Once you are familiar with these features in Figure 3.10 (see also Netter 108A, 108B, 109A, and 109B), try preparing yourself for lab by working through the Sylvius Self-Study Exercise—Medullary Surface (blue box below).
Chart 2-2 below lists these features and provides some additional localizing information. Once you are familiar with these features in Figure 3.2 (see also Netter 108A, 108B, 109A, and 109B) try working through the Sylvius Self-Study Exercise - Medullary Surface (blue box below)
| Chart 2-2 |
Ventral surface of medulla |
Dorsal surface of medulla |
Abducens nerve (VI)
medial of three nerves to emerge at junction of pons and medulla |
Fourth ventricle
caudal recess is visible in brainstem model/illustration; normally covered by cerebellum |
Facial nerve (VII)
middle of three nerves to emerge at junction of pons and medulla |
Gracile tract
pair of extended longitudinal bulges on either side of a deep midline furrow; technically, the name of the bulge is tuberculum gracilis, which is formed by the underlying gracile tract – the same tract of the dorsal spinal cord |
Vestibulocochlear nerve (VIII)
most lateral of three nerves to emerge at junction of pons and medulla |
Cuneate tract
pair of extended longitudinal bulges just lateral to the gracile tracts; technically, the name of the bulge is tuberculum cuneatus, which is formed by the underlying cuneate tract – the same tract of the dorsal spinal cord |
Inferior Olive
Pair of elongated bulges just lateral to the pyramids; a shallow furrow separates the pyramid and olive on each side of the medulla |
|
Glossopharyngeal nerve (IX)
most superior of a set of nerve roots that emerge just lateral to the olive and just caudal to the junction of the pons and medulla |
|
Vagus nerve (X)
middle of a set of nerve roots that emerge just lateral to the olive and slightly caudal to the junction of the pons and medulla |
|
Accessory nerve (XI)
most inferior of a set of nerve roots that emerge from the upper cervical spinal cord just lateral and caudal to the olive |
|
Hypoglossal nerve (XII)
nerve that emerges between the medullary pyramid and the olive |
|
Medullary pyramids
pair of extended longitudinal bulges on either side of a deep midline furrow |
|
Inferior olive
pair of elongated bulges just lateral to the pyramids; a shallow furrow separates the pyramid and olive on each side of the medulla |
|
Sylvius Self-Study Exercise—Medullary surface (click here to launch Sylvius online)
To explore the surface of the medulla when the brain is not in hand, open Sylvius4, enter the Brainstem Model in the Surface Anatomy group, and select Brainstem Model. This module will allow you to mouse-over each of the structures identified for you in the accompanying chart (above).
Once in the Brainstem Model module, click on a structure; when you do so, that structure becomes selected and a brief overview of that structure becomes available in the text window.
Tip—click on the loudspeaker icon at the bottom of the text window to hear the proper pronunciation of any term that is unfamiliar to you.
Take some time to explore these external features, working your way across one surface view and then the next. After familiarizing yourself with these standard ventral and dorsal views, click on the folder in the navigation window to the left and open the “interactive brainstem rotation” feature, which is a rotatable brainstem model. This feature will allow you to find these same structures in different longitudinal views of this standard brainstem model. Spend some time examining this model and comparing its surface features with those illustrated in Figure 2.9 (see also Netter 108A, 108B, 109A, and 109B).
Now that you have increased your familiarity with the surface features of the medulla in idealized representations of this brainstem division, find as many of features as you can in the photographic view of the ventral surface of the autopsy specimen. Enter the Photographic Atlas in the Surface Anatomy group, select Unlabeled and view the ventral surface of the brain.
Tip—to increase the magnification of the image, grab the lower-right corner of the image window and pull the window to its maximum extent; this should allow you to see several of the features identified in Figures 2.9, 2.10, and 2.11.
Unfortunately, the process of removing the brain from the cranium at autopsy usually results in the tearing of the smaller cranial nerve roots, so you will not see all of the cranial nerves that were once attached to the medulla in this view. Nevertheless, which cranial nerves do you see? The roots of which specific nerve(s) do you think are visible at the lateral junction of the pons and medulla? Can you distinguish the medullary pyramids from the inferior olives? Do you see the longitudinal furrow the separates these features? Remember which cranial nerve exits along this furrow?
Careful review of this Sylvius Self-Study exercise (and the following two exercises) will prepare you well for the most difficult phase of understanding brainstem neuroanatomy: recognizing the relation between surface features of the brainstem subdivisions and the internal structures that become evident when the each subdivision is sectioned transversely. Additional exercises will direct your conquest of this ultimate challenge in brainstem neuroanatomy. |
The pons
- Learning objective: to recognize the principal features of the pons as seen from the surface, including
the attachments of cranial nerves V and VI-VIII.
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.10 and its corresponding chart (Chart2-3).
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated just as easily in hemi-brains that were sectioned in the mid-sagittal plane. You
may wish to refer the actual specimens to the models available in the lab for comparison and/or to
the brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Pontine Surface).
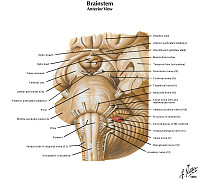
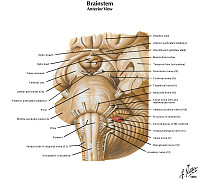
Now let’s examine the surface features of the middle subdivision of the brainstem, the pons.
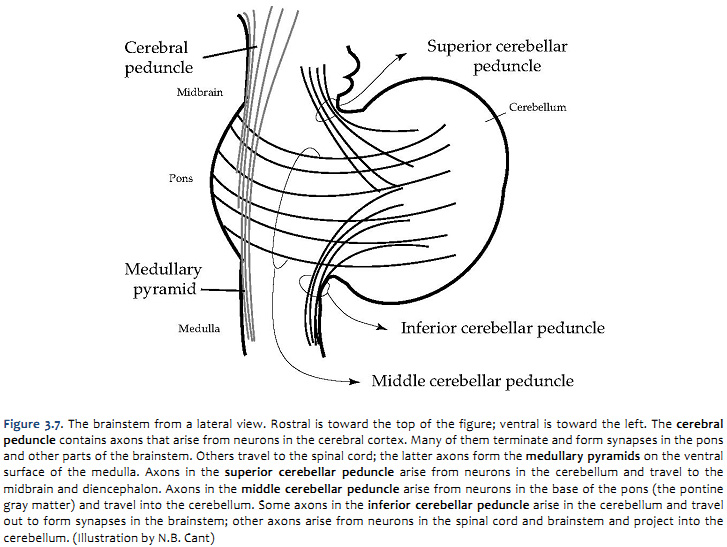
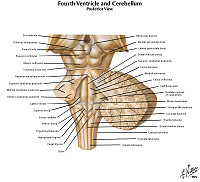
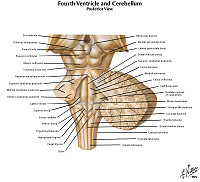
The pons is bounded caudally by the medulla and rostrally by the midbrain. The cerebellum is attached to its dorsal surface. Figure 2.10 (see also Netter 108A, 108B, 109A, and 109B)illustrates the key features of the pons that are visible on its external ventral surface and highlights important structures that are evident after removal of the cerebellum. These features include the massive system of transverse fibers on the ventral and lateral surface of the pons that give this subdivision its name (pons means “bridge”). These transversely coursing axons arise from neurons in the pons known as the pontine gray matter. The axons terminate in the cerebellum; their function will be considered in later sessions of the course.
The ventral surface of the pons also presents cranial nerves V-VIII, with nerves VI, VII & VIII attached to the brainstem at the junction of the medulla and the pons. As discussed above, cranial nerves VI-VIII are more properly associated with the pons, since these nerves originate or terminate in cranial nerve nuclei that are mostly localized to the caudal pons. Therefore, in the interest of helpful redundancy, these three nerves are listed again in chart 2-3, which also provides some additional localizing and structural information that you should appreciate. The most lateral of these three nerves is cranial nerve VIII, the vestibulocochlear nerve. Medial to it (and in a line with the exit point of nerves IX, X, and XI) is cranial nerve VII, the facial nerve. The most medial (in a line with the exit point of XII) is cranial nerve VI, the abducens nerve. Rostral to these nerves is cranial nerve V, the trigeminal nerve, which appears to plunge right into the fibers traversing the basal surface of the pons.
The dorsal surface of the pons is normally covered by the cerebellum, which is attached to it by three stalks or peduncles, the superior, middle, and inferior cerebellar peduncles (also, see Figure 2.14). Figure 2.10 illustrates the cut surfaces of the peduncles that are visible when the cerebellum is removed. The middle peduncle is continuous with the bridge of transverse pontine fibers on the basal surface and is carrying information into the cerebellum. The superior peduncle carries information away from the cerebellum toward the midbrain and thalamus (there is a minor afferent component to this peduncle that we will ignore in this course). The inferior peduncle contains axons traveling in both directions, connecting the cerebellum with the medulla and spinal cord. When the cerebellum is removed, the floor of the fourth ventricle is exposed. Two prominent bumps in the floor indicate the underlying nucleus of cranial nerve VI (the abducens nucleus).
Once you are familiar with these features in Figure 2.10, try working through the Sylvius Self-Study Exercise—Pontine Surface (blue box below).
| Chart 2-3 |
|
Ventral surface of pons |
Dorsal surface of pons |
Trigeminal nerve (V)
large nerves that penetrate the transverse fibers of the ventral-lateral pons |
Fourth ventricle
caudal recess is visible in mid-sagittal plane or in brainstem model/illustration; normally covered by cerebellum |
Abducens nerve (VI)
medial of three nerves to emerge at the junction of the pons and medulla |
Superior cerebellar peduncle
removal of the cerebellum requires a dorsal section of this cerebellar peduncle in a region where all three unite to form one large “stalk”; this peduncle conveys efferent axons from the cerebellum to the brainstem and thalamus |
Facial nerve (VII)
middle of three nerves to emerge at the junction of the pons and medulla |
Middle cerebellar peduncle (transverse fibers)
removal of the cerebellum requires a dorsal-lateral section of this largest of the cerebellar peduncles in a region where all three unite to form one large “stalk” |
Vestibulocochlear nerve (VIII)
most lateral of three nerves to emerge at the junction of the pons and medulla |
Inferior cerebellar peduncle
this peduncle conveys afferent axons from the spinal cord and brainstem to the cerebellum, as well as efferent axons from the cerebellum back to the brainstem |
Middle cerebellar peduncle (transverse fibers)
the pons is so-named because of a massive system of transverse fibers that “bridge” the longitudinal axis of the brainstem; these fibers originate in the basal region of the pons and continue around its ventral-lateral aspect to enter the contralateral cerebellar hemisphere |
|
Mnemonic note: the nerves with a roman numeral X in their name enter and exit at the medulla, those with a "V" (except IV) enter and exit the pons. |
Sylvius Self-Study Exercise—Pontine surface (click here to launch Sylvius online)
To explore the surface of the pons when the brain is not in hand, open Sylvius4, enter the Brainstem Model in the Surface Anatomy group, and select Brainstem Model. This module will allow you to mouse-over each of the structures identified for you in the accompanying chart on the previous page.
Following the same instructions provided in the previous Self Study Exercise in this Chapter to explore the brainstem model in static view, as well as the dynamic model in the “Atlas extras” folder. Spend some time examining this model in these two modes and comparing its surface features with those illustrated in Figure 3.11 (see also Netter 108A, 108B, 109A, and 109B)
Now that you have an increased familiarity with the surface features of the pons in idealized representations of this brainstem division, try to find as many of these features as you can in the photographic view of the ventral surface of the autopsy specimen. Enter the Photographic Atlas in the Surface Anatomy group, select Unlabeled and view the ventral surface of the brain. You will probably want a better view than the image that first opens so grab the lower-right corner of the image window and pull the window to its maximum extent; this should allow you to see several of the features listed in the chart on the previous page. You should now be able to appreciate the transverse fibers that dominate the ventral-lateral surface of the pons and the prominent trigeminal nerves that penetrate them.
Although this exercise is aimed at surface anatomy, view the image of the hemisected brain in the mid-sagittal plane (click on the thumbnail view of the Midsagittal brain in the Navigator window to the left). Note how the fourth ventricle occupies the space between the pons and the cerebellum. Note also the large bulbous expanse of neural tissue that accounts for the ventral pons; you are now looking into the complex intermingling of gray matter (pontine nuclei) and white matter (transverse fibers) that account for the communication of “command” signals from the cerebral cortex to the cerebellum (much more on that later in the course). If you look carefully, you will also note wisps of longitudinal white matter that run through this bulbous expanse in the ventral pons; these are fibers of the corticospinal tract that eventually coalesce into the medullary pyramids (again, much more on this critical pathway in a later session).
|
The midbrain
- Learning objective: to recognize the principal features of the midbrain as seen from the surface,
including the attachments of cranial nerves III & IV.
- Specimens: whole brains, mid-sagittal hemispheres, and brain or brainstem models
- Activities:
- Refer to Figure 2.11 and its corresponding chart (Chart2-4).
- Find each of the features listed in the chart and described in the text as you can on actual specimens
of the human brainstem. Some features may be best observed in whole brain specimens, but some
may be appreciated best in hemi-brains that were sectioned in the mid-sagittal plane. You may wish
to refer the actual specimens to the models available in the lab for comparison and/or to the
brainstem model in Sylvius4 Online (see the Sylvius Self-Study Exercise—Midbrain Surface).
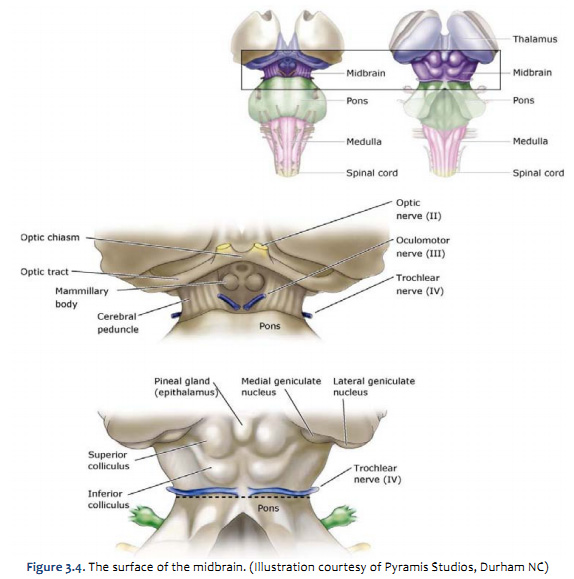  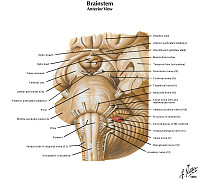  
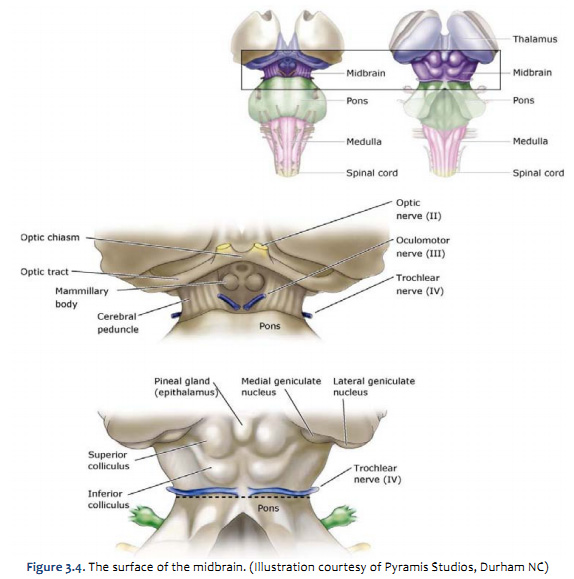
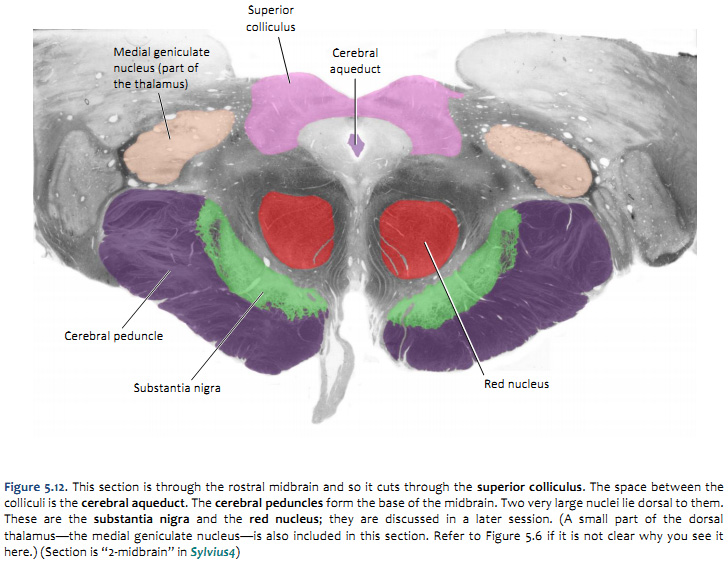
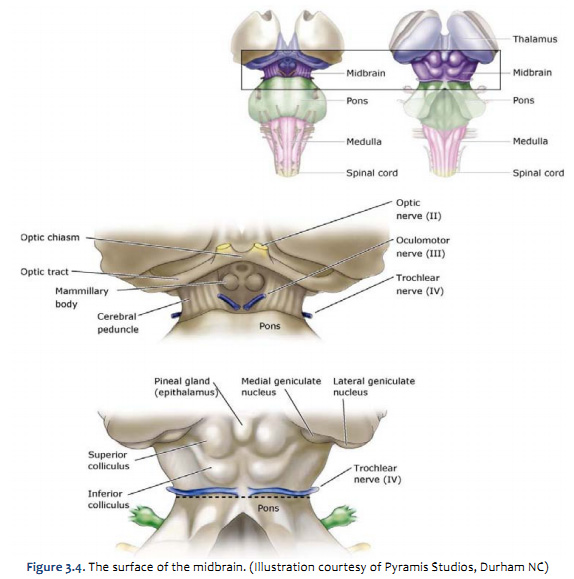
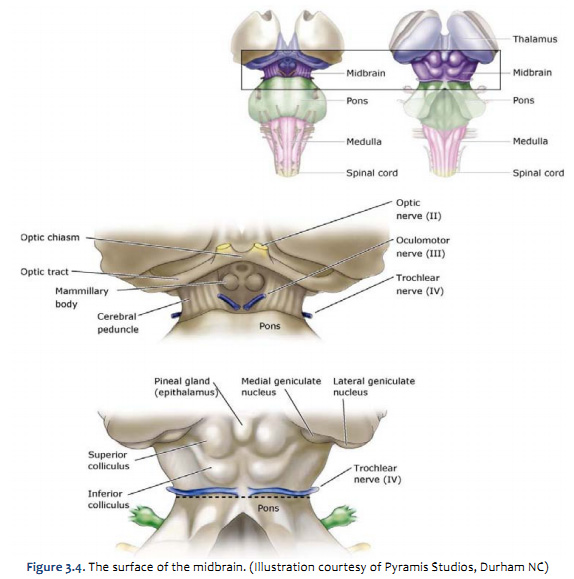
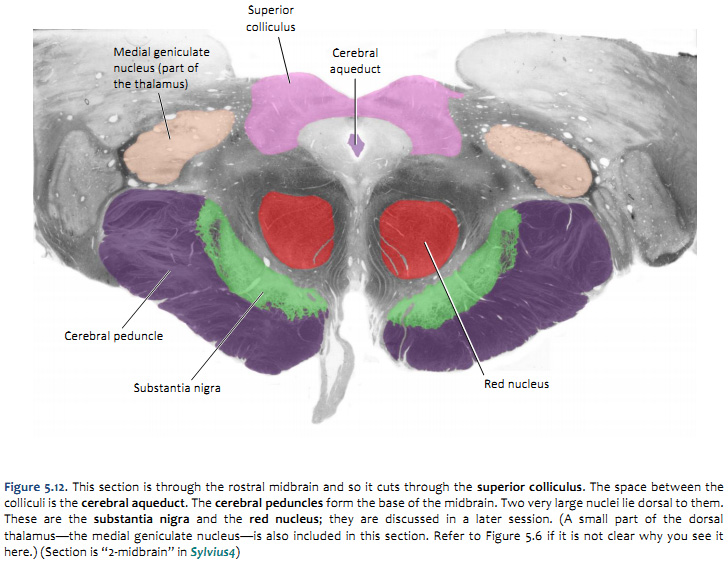
Let’s next examine the surface features of the superior subdivision of the brainstem, the midbrain (also commonly identified by its embryological name, the mesencephalon. It is bounded caudally by the pons and rostrally by the diencephalon, with which the boundary is somewhat vague. Figure 2.11 (see also Netter 108A, 108B, 109A, and 109B) illustrates the key features of the midbrain that are visible on its external ventral surface and highlights important structures that are evident on the dorsal surface after removal of the cerebellum. These features include the massive stalks of longitudinal fibers on the ventral-lateral surface of the midbrain, as well as cranial nerves III & IV. The chart below lists these features and provides some additional localizing and structural information that you should appreciate.
The massive fiber bundles known as the cerebral peduncles dominate the ventral surface of the midbrain. Strictly speaking, the term ‘cerebral peduncle’ refers to the entire basal portion of the midbrain; including the fiber bundles on the surface and everything dorsal to them up to the cerebral aqueduct. The fiber bundle on the surface should be called the pes pedunculi, or foot of the peduncle. However, for simplicity, in this Laboratory Guide, the term ‘cerebral peduncle’ will be used to refer to the fiber bundle. An indentation or space between the peduncles is known as the interpeduncular fossa. Cranial nerve III, the oculomotor nerve, emerges from the midbrain into this space between the peduncles.
On the dorsal surface, there are four bumps or colliculi (see also Netter 109A and 109B). The superior colliculus is concerned with orientation to visual (and other) stimuli. The inferior colliculus is part of the ascending auditory pathways. The pineal gland appears to form a fifth bump on the surface of the midbrain, but it is actually attached to the epithalamus of the diencephalon. Cranial nerve IV, the trochlear nerve, is the only cranial nerve that exits from the dorsal surface of the brain, and it is the set of only somatic motor efferents that innervates contralateral musculature. The trochlear nerve emerges at the border of the pons and midbrain, caudal to the inferior colliculus.
Did you realize that all other somatic motor components of
both cranial nerves and spinal nerves—except the trochlear
nerve—innervate ipsilateral musculature? So the trochlear
nerve is unsual in these two respects:
1) it exits the CNS from the dorsal aspect; and
2) it supplies contralateral muscles. |
Ventral surface of midbrain |
Dorsal surface of midbrain |
Cerebral peduncles
large, longitudinal “stalks” on the ventral-lateral aspect of the midbrain; their ventral portion—specifically, the basis pedunculi—consists of efferent fibers of the cerebral cortex that terminate in the brainstem and spinal cord |
Superior colliculi
superior pair of the four bumps that are visible in brainstem model/illustration; normally covered by cerebellum |
Interpeduncular fossa
external space between the cerebral peduncles |
Inferior colliculi
inferior pair of the four bumps that are visible in brainstem model/illustration; normally covered by cerebellum |
Oculomotor nerve (III)
nerves that emerge from the interpeduncular fossa, just medial to the cerebral peduncles |
Trochlear nerve (IV)
visible in brainstem model/illustration; normally covered by cerebellum; exits from the dorsal surface of the brainstem |
Now, try working through the Sylvius Self-Study Exercise - Midbrain Surface (blue box below).
Sylvius Self-Study Exercise—Midbrain surface (click here to launch Sylvius online)
To explore the surface of the midbrain when the brain is not in hand, open Sylvius4, enter the Brainstem Model in the Surface Anatomy group, and select Brainstem Model. This module will allow you to mouse-over each of the structures identified for you in the accompanying chart on the previous page.
Following the same instructions provided in the previous two Self Study Exercises in this Chapter to explore the brainstem model in static view, as well as the dynamic model in the “Atlas extras” folder. Spend some time examining this model in these two modes and comparing its surface features with those illustrated in Figure 3.4 (see also Netter 108A, 108B, 109A, and 109B).
Now that you have an increased familiarity with the surface features of the midbrain, try to find as many of these features as you can in the photographic view of the ventral surface of the autopsy specimen. Enter the Photographic Atlas in the Surface Anatomy group, select Unlabeled and view the ventral surface of the brain. Again, you should grab the lower-right corner of the image window and pull the window to its maximum extent, which will allow you to see several of the features listed in the chart on the previous page. You should now be able to appreciate both the cerebral peduncles and the interpeduncular fossa. Note the paired bumps that reside just medial to the cerebral peduncles where they disappear into the base of the forebrain; what are these bumps and in which embryological subdivision of the CNS are they located?
Although this exercise is aimed at surface anatomy, another quick review of the hemisected brain in the mid-sagittal plane is worth a minute to reinforce the relation between ventricular compartment and embryological subdivision. The ventricular system achieves its narrowest constriction in the adult CNS in the midbrain; in this view, you can easily appreciate this fact as you recognize the cerebral aqueduct. Here’s a study tip for future lessons in sectional anatomy: whenever you see the cerebral aqueduct, you are looking at the midbrain, regardless of the plane of section. More generally, whenever confronted with a sectional view of the CNS, look first for ventricular compartments; they will quickly cue you as to what division of the CNS you are investigating. Finally, what do you see above the cerebral aqueduct in this image? This portion of the midbrain is also called the tectum, which means “roof” (the tectum forms the roof of the cerebral aqueduct).
|
The brainstem is put back together in unlabeled Figures 2.12 and 2.13. Make sure that you can identify all of the structures (in bold) discussed in this chapter up to this point.
 
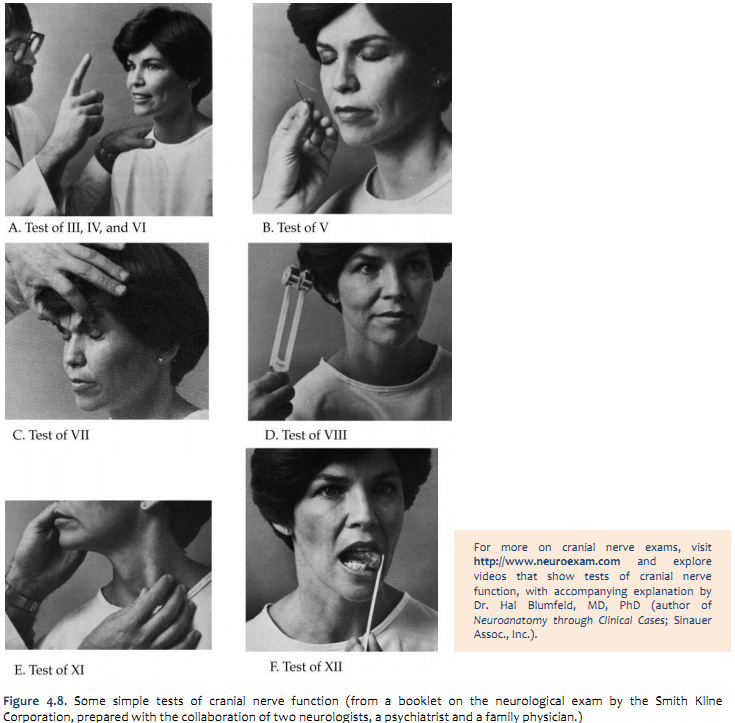
Review of cranial nerves and their primary functions

One means for reinforcing your understanding of the functional significance of the cranial nerves that you have just reviewed is to actually test their functions in yourself and your teammates. You will do this as you learn the neurological component of the physical examination in the Practice course. For our purposes here, simply refer to table A2 (from Purves et al., Neuroscience, 5th Ed., Sinauer Assoc., Inc.) and then consider the means by which you would assess the functional integrity of the cranial nerves. Actually, there are a number of tests of cranial nerve function that can be done with very simple materials. These tests provide considerable information about the presence or absence of normal function in the brainstem and the nerves themselves. You should appreciate how such simple tests can be used clinically and why a foundational understanding of functional neuroanatomy is critical for interpreting the findings from such functional assessments.
Cranial nerves III, IV, and VI
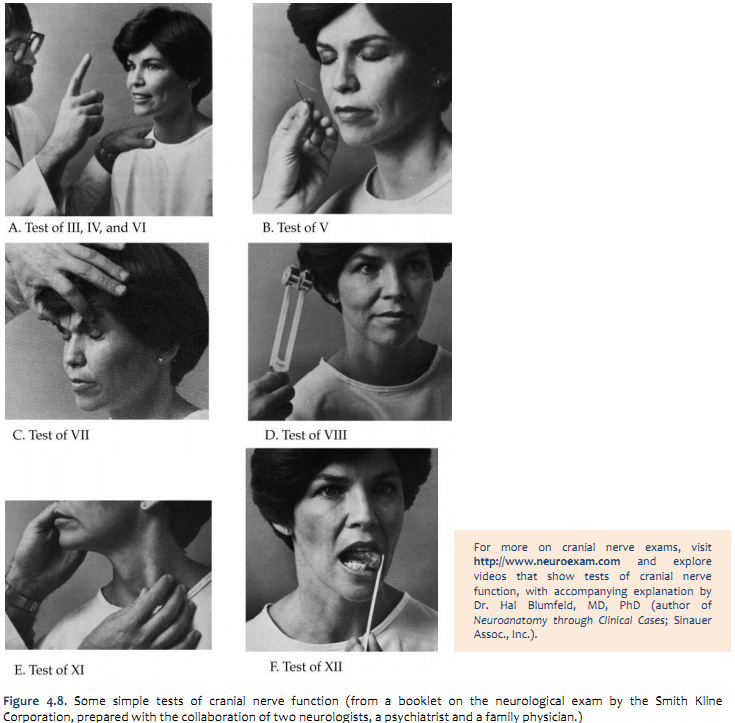
These nerves are tested as a unit, since all supply muscles for eye movement. The oculomotor nerve also supplies the levator muscle that elevates the lids and the smooth muscles that constrict the pupils. Range of ocular movement is checked by asking the patient to follow the movements of the examiner’s fingers as they are moved in all directions of gaze (Figure 3.8A). With involvement of the oculomotor nerve, the patient will not be able to look up, down or medially with the affected eye. There will also be dilation of the pupil and droopiness (ptosis) or closure of the lid on the affected side. If the trochlear nerve is affected, the patient will be unable to look downward when the eye is adducted. If the abducens nerve is affected, the patient will not be able to look laterally with the involved eye. In any of these cases, the patient may complain of double vision. (It is important to remember that either the nerves themselves or their nuclei in the midbrain and pons may be involved.) Examination of the pupillary reflexes involving nerves II and III will be explored in a later course session.
Cranial nerve V
The examiner first checks for the presence of the several types of sensation and then determines whether both sides of the face are equally sensitive. Failure to feel wisps of cotton touching the forehead, cheeks and jaw indicates anesthesia to light touch. Differences in response on the two sides of the face indicate increased or decreased sensitivity to light touch. The same procedure is followed in testing for degree of sensitivity to pinpricks (see Figure 3.8B) and to warm and cold objects.
The masseter and temporal muscles (muscles of mastication innervated by the motor component of the fifth nerve) are examined by palpating them when the jaws are clamped tightly together. The examiner should note whether there is deviation of the jaw when the mouth is opened.
Cranial nerve VII
The patient is asked to imitate the examiner as he or she looks at the ceiling, wrinkles the forehead, frowns, smiles, shows teeth, and raises the eyebrows. Any asymmetry of the face is noted. To test the strength of the eyelid muscles, the patient is asked to keep his or her eyes closed while the examiner attempts to open them (Figure 3.8C). The sensory portion of the facial nerve can be tested by having the patient identify the taste of sugar and salt placed on the anterior part of the tongue on each side.
Cranial nerve VIII
The eighth nerve is divided into two parts, the cochlear or auditory nerve and the vestibular nerve. Special equipment is required to examine the vestibular nerve and it is not tested routinely. (If the patient gives a history of vertigo or disturbed balance, the possibility of a vestibular nerve lesion should be considered and the patient can be given a caloric test, which is described in Purves et al., Neuroscience 5th Ed., Chapter 14, Box 14C.) Preliminary tests of hearing can be done with a tuning fork (Figure 3.8D), but detailed auditory testing is done by an audiologist.
Cranial nerves IX and X
The pharyngeal gag reflex is tested by touching each side of the pharynx with a tongue depressor or applicator stick. The palatal reflex is tested by stroking each side of the mucous membrane of the uvula. The side touched should rise. Normal function of the vagus nerve is revealed by the patient’s ability to swallow and to speak clearly without hoarseness, by symmetrical movements of the vocal cords, and by symmetrical movements of the soft palate when he or she says “Ah.”
Cranial nerve XI
The examiner 1) palpates and notes the strength of the trapezius muscle while the shoulders are shrugged against resistance, and 2) palpates and tests the sternocleidomastoid muscle for strength (Figure 3.8E).
Cranial nerve XII
Any lateral deviation of the tongue when it is protruded is noted. The examiner also looks for atrophy or tremor of the tongue. The strength of the tongue is tested by asking the patient to protrude it and to move it from side to side against a tongue depressor (Figure 3.8F).
For more on cranial nerve exams, visit http://www.neuroexam.com and explore videos that show tests of cranial nerve function, with accompanying explanation by Dr. Hal Blumfeld, MD, PhD (author of Neuroanatomy through Clinical Cases; Sinauer Assoc., Inc.). |
The Peduncles
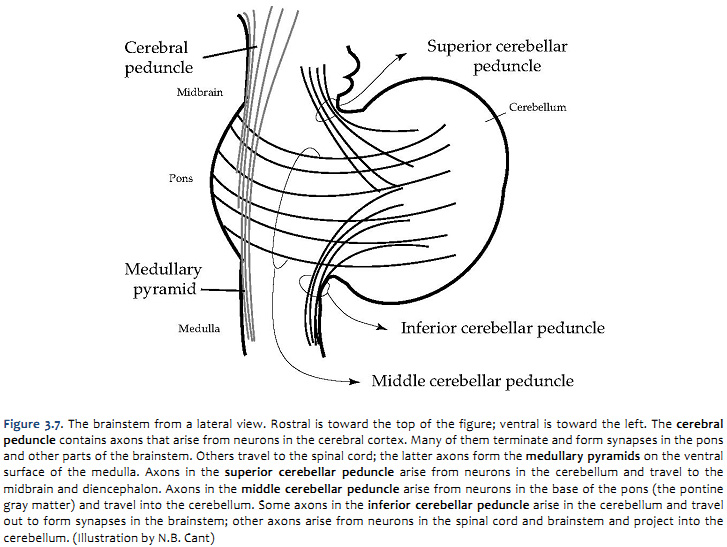
The four fiber bundles referred to as ‘peduncles’ are illustrated in a simplified drawing in Figure 2.14. The functions of these fiber bundles are considered in later course sessions. For now, it is sufficient to learn the difference between the cerebral and cerebellar peduncles and their locations in the brainstem. You have already been introduced to these peduncles; now use Figure 2.14 to understand the spatial relations among the peduncles, and to reinforce your knowledge of their relations to the subdivisions of the central nervous system they interconnect.
The internal anatomy of the brainstem
The internal organization of the brainstem is considerably more complicated than that of the spinal cord. However, two factors work in your favor as you study its features. First, important general principles of organization of the spinal cord also hold true for the brainstem. Second, much of the complexity of the brainstem is contributed by cell groups and axon tracts that will not be considered in this course. In the following discussion, the general plan of organization of the brainstem is presented first. Next, the prominent internal features that characterize each subdivision are identified. In the next laboratory session, we will focus on the cranial nerve nuclei and a set of neuromodulatory nuclei that will figure prominently in discussions during the “behavioral science” side of our course on Brain and Behavior. An understanding of the functions and locations of these nuclei is essential for diagnosing (and treating) neurological injury, dysfunction and disease, as well as mental illness and a spectrum of dysfunctions manifest in human behavior.
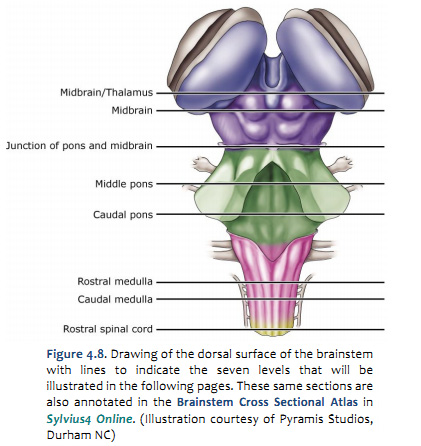
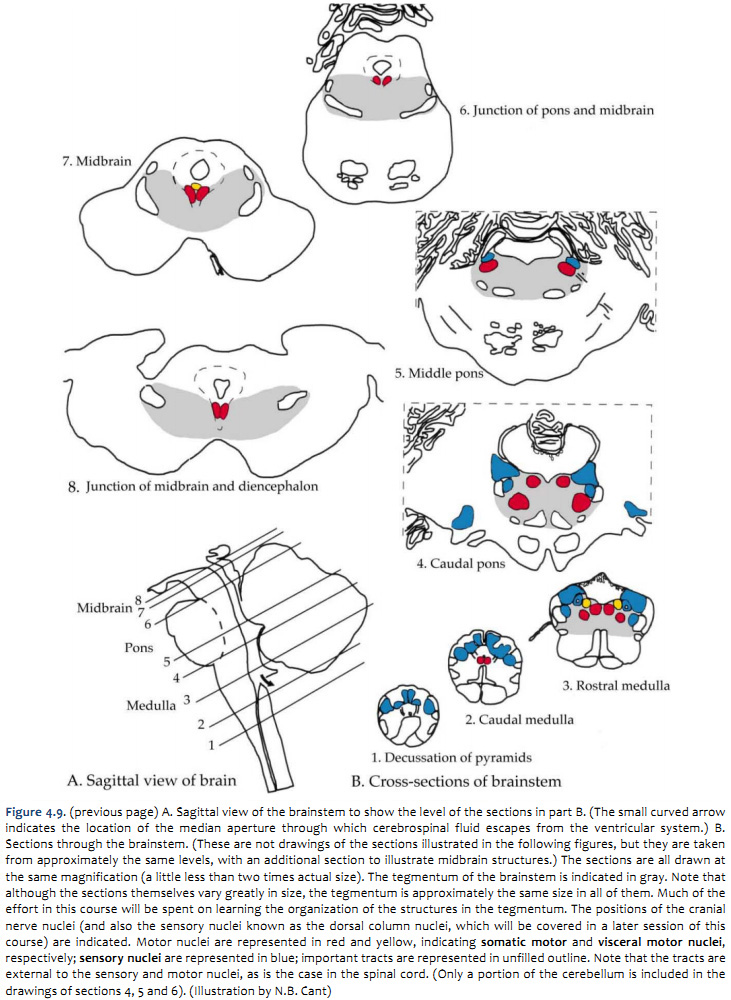
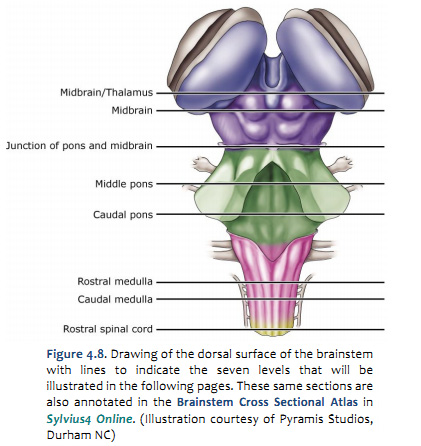
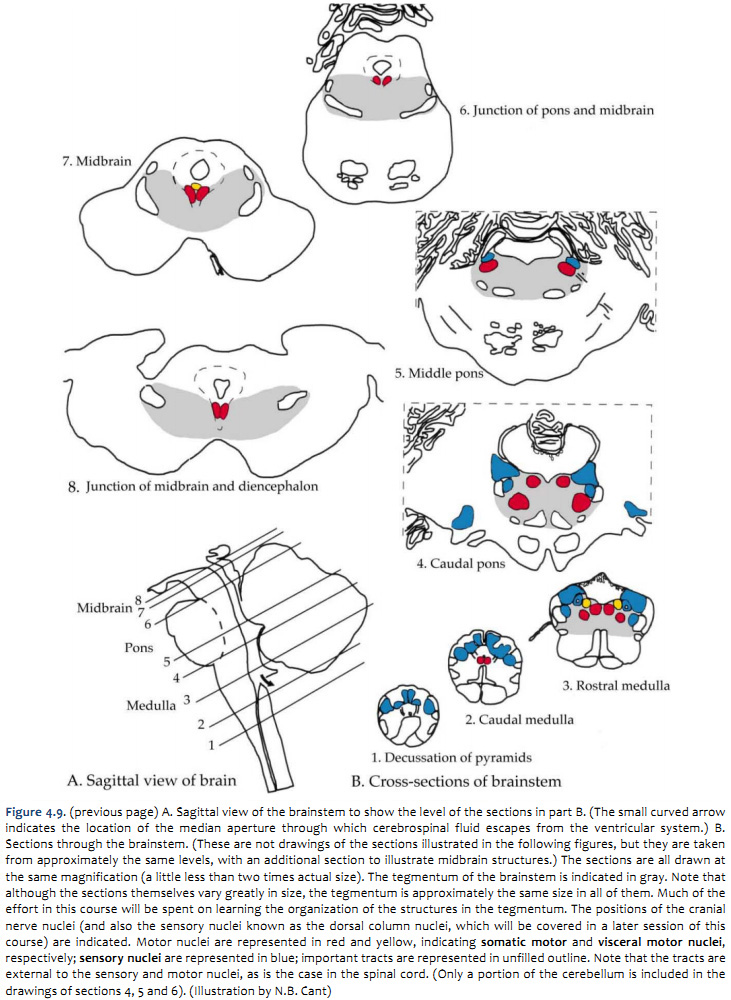
It would be convenient if each subdivision of the brainstem were sufficiently homogeneous along its length that one cross-section could serve as a ‘typical’ representative for the entire subdivision. However, the brainstem changes continuously along its length—the subdivision into three parts is somewhat arbitrary. As a compromise between examining three sections (one for each subdivision) and hundreds, seven sections of the brainstem are shown to serve as representatives (Figure 2.15).
Once you understand the organization of these seven levels and the way various pathways traverse them, you should be able to identify the location of any section through the brainstem and the important pathways represented in it.
A schematic overview of the levels of the brainstem to be discussed is presented in Figure 4.9. At this stage, it is not important to study the details; we will come back to them. For now, three points should be taken from the figure:
- All of the sections are shown at the same magnification. In most atlases (including Sylvius4 Online), the smaller sections are magnified more than the larger ones, and it is easy to lose sight of the relative proportions of the different subdivisions.
- The cranial nerve nuclei lie in the tegmentum of the brainstem, as do many of the major ascending and descending tracts.
- Just as in the spinal cord, the nuclei that receive sensory inputs via the cranial nerves are spatially separate from those that give rise to motor output. The sensory nuclei are located laterally in the brainstem, whereas the motor nuclei are located medially. The spatial segregation of sensory and motor functions provides an important clue for localization of focal damage in the brainstem.
In Figures 2.16, 2.17, 2.18, 2.19, 2.20, 2.21, major landmarks in each of the subdivisions are identified in sections
prepared to enhance the appearance of myelin (again, it is conventional to prepare sections of the brainstem and spinal
cord with stains that make the white matter appear dark). As usual, be sure to focus on the structures identified in the figure legends in bold font. Our purpose here is to help you recognize the distinctive features of the embryological subdivisions of the brainstem, and to introduce you to some of the gray matter (nuclei) and white matter (tracts; peduncles) that you will study in more detail elsewhere in the course. We will return to these same sections frequently as the course progress (these same section are fully annotated in Sylvius4 Online), including the next laboratory session when we will turn our attention squarely on the cranial nerve and neuromodulatory nuclei.
Sylvius Self-Study Exercise—Internal Brainstem Features (click here to launch Sylvius online)
The Brainstem Cross Sectional Atlas in Sylvius4 contains 14 sections through the brainstem and four spinal cord sections featuring segmentation of well over 100 neuroanatomical structures. This atlas should be used to fill-in the gaps between the seven sections illustrated in this chapter.
As you work through these chapter figures and the associated legends, find the same structures one at a time in the Brainstem Cross Sectional Atlas in Sylvius4. The sections shown here are actually re-colorized versions of the same sections that are in Sylvius4. As suggested in Lab 1, you may wish to look-up each labeled term (and each term that appears in bold in the figure legends) in the Sylvius4 Visual Glossary module; there, you can ‘bookmark’ each term for further study and review.
Since we are not yet studying the functional significance of many of these structures (we will do so over the next few weeks), you should click on the structures identified in the figures, and when you do so, that structure becomes selected and a brief overview of that structure becomes available in the text window.
Tip—click on the loudspeaker icon at the bottom of the text window to hear the proper pronunciation of any term that is unfamiliar to you.
Tip—to increase the magnification of the image, grab the lower-right corner of the image window and pull the window to its maximum extent.
|
| Challenge 2.2—internal anatomy of the medulla
 
With reference to Figures 2.16, 2.17, and the chart below, carefully inspect the internal features of the medulla from its caudal union with the spinal cord to the pons. Spend some time browsing the six medullary sections in Sylvius4, and find each of the internal features described in the chart below.
Subdivision |
Surface feature |
Internal structure |
Caudal medulla
(Figure 2.16) |
Gracile tract
(dorsal surface)
- pair of extended longitudinal bulges on either side of a deep midline furrow; technically, this bulge is called the tuberculum gracilis, which is formed by the underlying gracile tract
- continuation of the tract of the dorsal spinal cord
|
Gracile tract & nucleus
- medial, superficial bundle of myelinated axons arising from the dorsal column of the spinal cord
- just deep to the gracile tract is the gracile nucleus, a compact gray matter structure that receives the synapses made by gracile tract axons
|
Cuneate tract
(dorsal surface)
- pair of extended longitudinal bulges just lateral to the gracile tracts; technically, this bulge is called the tuberculum cuneatus, which is formed by the underlying cuneate tract
- continuation of the tract of the dorsal spinal cord
|
Cuneate tract & nucleus
- just lateral to the gracile tract, superficial bundle of myelinated axons arising from the dorsal column of the spinal cord
- at the superior “head” of the cuneate tract is the cuneate nucleus, a compact gray matter structure that receives the synapses made by cuneate tract axons
|
Pyramidal decussation
(ventral surface)
- see Medullary pyramids below
- apparent “stitching” of fibers that cross the midline
|
Pyramidal decussation
- see Medullary pyramids below
- midline crossing of dense bundles of myelinated axons that run the longitudinal extent of the ventral brainstem
- accounts for the formation of the lateral and ventral (anterior) corticospinal tracts of the spinal cord
|
Middle to rostral medulla
(Figure 2.17) |
Medullary pyramids
(ventral surface)
- pair of extended longitudinal bulges on either side of a deep midline furrow
|
Medullary pyramids
- dense bundle of myelinated axons that run the longitudinal extent of the ventral brainstem; these axons are also known as the corticospinal tract
- these same axons are present in the internal capsule, cerebral peduncles, basilar pons, and about 90% are present in the lateral columns of the spinal cord
|
Inferior olive
(ventral-lateral surface)
- pair of elongated bulges just lateral to the pyramids; a shallow furrow separates the pyramid and olive on each side
|
Inferior olivary nucleus
- prominent nucleus of the ventral-lateral medulla just dorsal to the medullary pyramids
- note the highly convoluted bands of gray matter that account for the superficial, ventral-lateral bulge
|
Hypoglossal nerve (XII)
(ventral-lateral surface)
- exits through ventral-medial surface
|
Hypoglossal nerve roots & nucleus
- nerve roots emerge between the medullary pyramid and the olive
- trace these nerve roots dorsally to their origin in the hypoglossal nucleus, located along the dorsal midline
|
|
| Challenge 2.3—internal anatomy of the pons
With reference to Figures 2.18, 2.19 and the chart on the following page, carefully inspect the internal features of the pons. As you did for the medulla, spend some time browsing the sections in Sylvius4, and find each of the internal features described in the chart below.
Subdivision |
Surface feature |
Internal structure |
Middle of pons
fig 2.18 |
Middle cerebellar peduncle
(ventral-lateral surface)
- massive system of transverse fibers that “bridge” the longitudinal axis of the brainstem; these fibers originate in the basal region of the pons and continue around its ventral-lateral aspect to enter the cerebellum
|
Pontocerebellar fibers & middle cerebellar peduncle
- the ventral half of the pons (also called the basilar pons) contains gray matter, longitudinal axons, and transverse fibers called the pontocerebellar fibers that decussate and form the contralateral middle cerebellar peduncle
- these fibers arise from a scattering of gray matter in the basilar pons, called the pontine nuclei, and terminate in the contralateral cerebellum
- also in the basilar pons are prominent fascicles of axons from the cerebral cortex that project to various nuclei of the brainstem and the spinal cord; collectively, these are the corticobulbar/corticospinal fibers
|
Trigeminal nerve (V)
(ventral-lateral surface)
- enters/exits pons by penetrating the transverse, pontocerebellar fibers
|
Trigeminal nerve roots & nucleus
- trace the nerve V roots dorsally to their origin in the trigeminal nuclear complex; at this level, note the location of the trigeminal motor nucleus and, just lateral to it, the principal (chief sensory) nucleus
- now, keep your eye in this same general region and section caudally: in this same dorsal-lateral position in the caudal pons and throughout the medulla, the spinal trigeminal nucleus and the spinal trigeminal tract are present (the spinal nucleus can be further subdivided)
|
Caudal pons
fig 2.19 |
Abducens nerve (VI)
(ventral-medial surface)
- enters/exits near the midline at the pontomedullary junction (most medial of the three that emerge from this junction)
|
Abducens nerve roots & nucleus
- explore the medial tegmentum of the pons and locate nerve VI roots; note how they course through the basilar pons just lateral to the corticobulbar/corticospinal fibers
- trace these nerve roots dorsally to their origin in the abducens nucleus, which is located along the dorsal midline
|
Facial nerve (VII)
(ventral-lateral surface)
- enters/exits through ventral-lateral surface at pontomedullary junction (middle of the three that emerge from this junction)
|
Facial nerve roots & nucleus
- explore the lateral tegmentum of the pons and locate nerve VII roots; note how they trace a most unusual trajectory around the dorsal aspect of the abducens nucleus (cf. figures 4.15 & 4.17)
- it may not be possible to trace these nerve roots all the way back to their origin in the facial nucleus, which is located just medial and ventral to the trigeminal nuclear complex
- nerve VII roots exit the facial nucleus medially, then course dorsally around the abducens nucleus, and finally ventral-laterally toward a lateral exit (this is how nerve VII ends up being lateral to nerve VI)
|
Vestibulocochlear nerve (VIII)
(ventral-lateral surface)
- enters through ventral-lateral surface at pontomedullary junction (most lateral of the three that emerge from this junction)
|
Vestibular nuclear complex
- explore the lateral tegmentum of the pons and locate nuclei of the vestibular nuclear complex (you may not find any nerve VIII roots in these cross sections); you will find the vestibular nuclei dorsal to the trigeminal nuclear complex and spinal trigeminal tract
- find the superior, lateral and medial vestibular nuclei
- section down into the medulla and locate the spinal vestibular nucleus
- so what about the cochlear division of nerve VIII? It terminates in a superficial nucleus of the dorsal-lateral upper medulla called the cochlear nucleus. Although not labeled in Sylvius4, it is visible in the section labeled “8-Medulla” as the gray matter that wraps around the dorsal-lateral surface of the inferior cerebellar peduncle
|
|
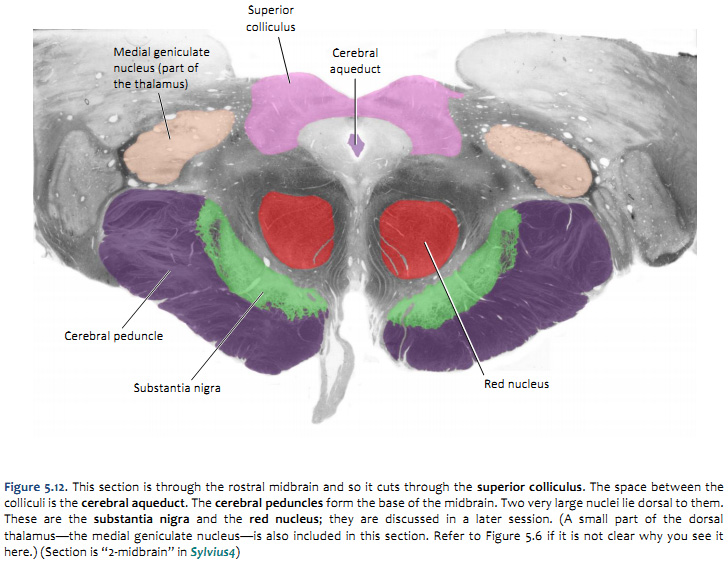
| Challenge 2.4—internal anatomy of the midbrain
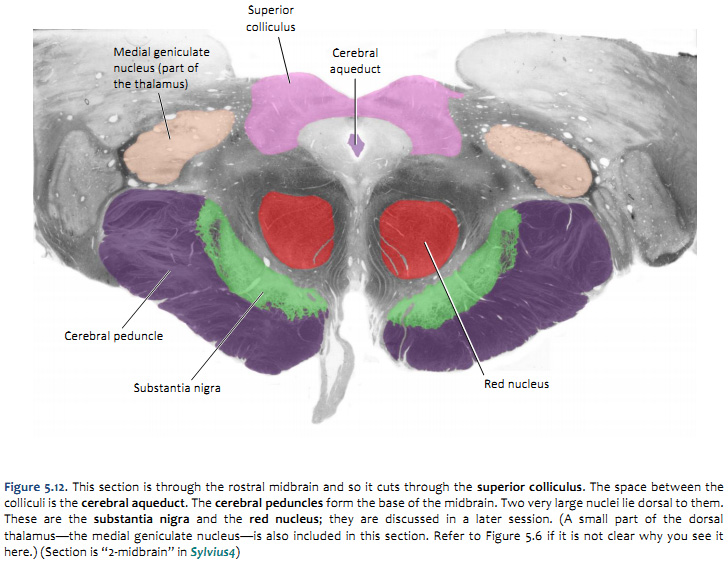 
With reference to Figures 2.20, 2.21, and the chart on the following page, carefully inspect the internal features of the midbrain. As you did for the medulla and pons, now spend some time browsing the sections in Sylvius4, and find each of the internal features described in the chart below. |
Subdivision |
Surface feature |
Internal structure |
Midbrain
(Figures 2.20 and 2.21) |
Cerebral peduncles
(ventral surface)
- large, longitudinal “stalks” (peduncle mean stalk) that occupy the ventral midbrain
|
Cerebral peduncles
- technically, “cerebral peduncle” refers to the entire ventral midbrain, including the midbrain tegmentum and the fiber systems that run through the stalks; however, it is common to use the term “cerebral peduncle” to refer specifically to these fiber systems (the proper term for these ventral portions of the peduncles—where the fibers are—is basis pedunculi)
- the cerebral peduncles comprise efferent fibers of the cerebral cortex that terminate in the brainstem and spinal cord; these fibers are referred to collectively as the corticobulbar / corticospinal fibers; this compound terms indicates that the some of these fibers terminate among brainstem nuclei (“bulbar” refers to the brainstem and cranial nerve nuclei), while other fibers continue through the brainstem and terminate in the spinal cord
- it is important to recognize the course of these fibers from their origin in the cerebral cortex through brainstem: cerebral cortex → subcortical white matter → internal capsule → cerebral peduncle → basilar pons → medullary pyramids → lateral and anterior (ventral) corticospinal tract
- there are about 20 million axons in each cerebral peduncle; can you guess how many axons are present in medullary pyramid by simply noting the difference in size of these two structures?1 (the majority of these axons never reach the spinal cord)
- now consider the tegmentum of the midbrain; just dorsal to the cerebral peduncles (basis pedunculi) there is an important gray matter nucleus called the substantia nigra, which you will learn much more about when we study the basal ganglia
- and just dorsal to the substantia nigra, is a spherical gray matter structure called the red nucleus, which you will study when we consider cerebellar systems
|
|
Oculomotor nerve (III)
(ventral surface)
- exits through ventral surface just medial to cerebral peduncles (in the interpenducular fossa)
|
Oculomotor nerve roots & nuclear complex
- trace these nerve roots dorsally to their origin in the nuclei of the oculomotor complex along the midline of the dorsal tegmentum; here you will find two divisions: the oculomotor nucleus and the Edinger-Westphal nucleus
- this nuclear complex is embedded within a large region of gray matter that surrounds the cerebral aqueduct, termed the periaqueductal (or central) gray
|
|
Inferior colliculi
(dorsal surface)
- inferior pair of the four bumps that are visible in brainstem model/illustration, but are normally covered by the cerebellum
|
Inferior colliculi
- in the caudal midbrain, the inferior colliculi are gray matter structures that occupy a position just dorsal and lateral to the periaqueductal gray (see section “3 - Midbrain”)
- together with the superior colliculi, they form the “roof” of the midbrain (above the cerebral aqueduct); for this reason, these four bumps are also called the tectum (tectum means roof)
- the trochlear nerve exits the dorsal surface of the brainstem just caudal to the inferior colliculus (see Brainstem Model in Surface Anatomy module)
- although that nerve is not visible in section 3 – Midbrain, you can see the small trochlear nuclei where you should expect to find somatic motor nuclei, along the midline of the dorsal tegmentum
|
|
Superior colliculi
(dorsal surface)
- superior pair of the four bumps that are visible in brainstem model/illustration, but are normally covered by cerebellum
|
Superior colliculi
- in the rostral midbrain, the superior colliculi are laminated gray matter structures that occupy a position just dorsal and lateral to the periaqueductal gray matter (see section lableled “2 - Midbrain”)
- together with the inferior colliculi, they form the “roof” (tectum) of the midbrain (above the cerebral aqueduct)
|
1There are about half a million axons in each medullary pyramid.
Examine slabs through human brainstem specimens
- Learning objective: to recognize the principal features of the brainstem that are visible with the unaided eye, including major gray matter and white matter structures in each embryological division.
- Specimens: whole brain slabs or gross sections cut through the brainstem
- Activities:
- Repeat Challenges 3.2−3.4 using gross sections through the human brainstem, referring to the charts and figures associated with the text and the Brainstem Atlas in Sylvius4 Online.
- Find as many of the visible gray and white matter features listed in the chart and described in the text as you can on actual specimens of the human brainstem.
|
Click here to submit questions or comments about this site.
Duke University | Duke Medicine | School of Medicine | School of Nursing | Doctor of Physical Therapy
Copyright © 2004-2016 Duke University School of Medicine
Updated 01/06/16 - Velkey |
|